DIABETIC RETINOPATHY
Diabetic retinopathy is a condition that may occur in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye.
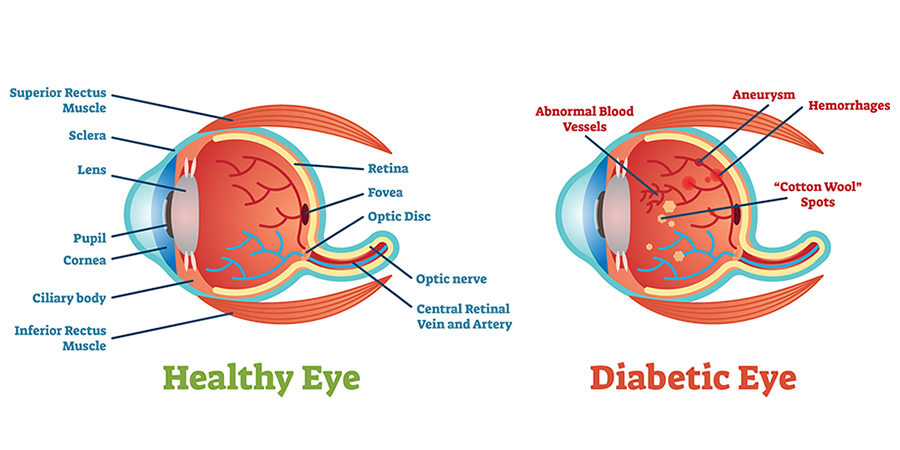
Diabetic retinopathy is a serious sight-threatening complication of diabetes. Diabetes interferes with the body’s ability to use and store sugar (glucose). The disease is characterized by too much sugar in the blood, which can cause damage throughout the body, including the eyes. Over time, diabetes damages small blood vessels throughout the body, including the retina. Diabetic retinopathy occurs when these tiny blood vessels leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision.
Diabetic retinopathy usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness. When people with diabetes experience long periods of high blood sugar, fluid can accumulate in the lens inside the eye that controls focusing. This changes the curvature of the lens, leading to changes in vision. However, once blood sugar levels are controlled, usually the lens will return to its original shape and vision improves. Patients with diabetes who can better control their blood sugar levels will slow the onset and progression of diabetic retinopathy.
According to a 2018 American Eye-Q ® survey conducted by the AOA, nearly half of Americans didn’t know whether diabetic eye diseases have visible symptoms (often which the early stages of diabetic retinopathy does not). The same survey found that more than one-third of Americans didn’t know a comprehensive eye exam is the only way to determine if a person’s diabetes will cause blindness, which is why the AOA recommends that everyone with diabetes have a comprehensive dilated eye examination at least once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
Causes & risk factors
Diabetic retinopathy results from the damage diabetes causes to the small blood vessels located in the retina. These damaged blood vessels can cause vision loss:
- Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
- In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
Diabetic retinopathy is classified into two types.
Non-proliferative diabetic retinopathy
Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or nonexistent. In NPDR, the blood vessels in the retina are weakened. Tiny bulges in the blood vessels, called microaneurysms, may leak fluid into the retina. This leakage may lead to swelling of the macula.
Proliferative diabetic retinopathy
Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease. At this stage, circulation problems deprive the retina of oxygen. As a result, new, fragile blood vessels can begin to grow in the retina and into the vitreous, the gel-like fluid that fills the back of the eye. The new blood vessels may leak blood into the vitreous, clouding vision.
Other complications of PDR include detachment of the retina due to scar tissue formation and the development of glaucoma. Glaucoma is an eye disease in which there is progressive damage to the optic nerve. In PDR, new blood vessels grow into the area of the eye that drains fluid from the eye. This greatly raises the eye pressure, which damages the optic nerve. If left untreated, PDR can cause severe vision loss and even blindness.
Risk factors for diabetic retinopathy include:
- Diabetes. People with type 1 or type 2 diabetes are at risk for developing diabetic retinopathy. The longer a person has diabetes, the more likely he or she is to develop diabetic retinopathy, particularly if the diabetes is poorly controlled.
- Race. Hispanics and African Americans are at greater risk of developing diabetic retinopathy.
- Medical conditions. People with other medical conditions, such as high blood pressure and high cholesterol, are at greater risk.
- Pregnancy. Pregnant women face a higher risk of developing diabetes and diabetic retinopathy. If a woman develops gestational diabetes, she has a higher risk of developing diabetes as she ages.
- Family History.
Symptoms
Symptoms of diabetic retinopathy include:
- Seeing spots or floaters.
- Blurred vision.
- Having a dark or empty spot in the center of your vision.
- Difficulty seeing well at night.
Diagnosis
Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with emphasis on evaluating the retina and macula, may include:
- Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be affecting vision.
- Visual acuity measurements to determine how much central vision has been affected.
- Refraction to determine if a new eyeglass prescription is needed.
- Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil.
- Measurement of the pressure within the eye.
Supplemental testing may include:
- Retinal photography or tomography to document the current status of the retina.
- Fluorescein angiography to evaluate abnormal blood vessel growth.
Treatment
Treatment of diabetic retinopathy varies depending on the extent of the disease. People with diabetic retinopathy may need laser surgery to seal leaking blood vessels or to discourage other blood vessels from leaking. A doctor of optometry might need to inject medications into the eye to decrease inflammation or stop the formation of new blood vessels. People with advanced cases of diabetic retinopathy might need a surgical procedure to remove and replace the gel-like fluid in the back of the eye, called the vitreous. Surgery may also be needed to repair a retinal detachment. This is a separation of the light-receiving lining in the back of the eye.
If you are diabetic, you can help prevent or slow the development of diabetic retinopathy by:
- Taking your prescribed medication.
- Sticking to your diet.
- Exercising regularly.
- Controlling high blood pressure.
- Avoiding alcohol and smoking.
Laser treatment (photocoagulation) is used to stop the leakage of blood and fluid into the retina. A laser beam of light can be used to create small burns in areas of the retina with abnormal blood vessels to try to seal the leaks. Treatment for diabetic retinopathy depends on the stage of the disease. The goal of any treatment is to slow or stop the progression of the disease. In the early stages of non-proliferative diabetic retinopathy, regular monitoring may be the only treatment. Following your doctor’s advice for diet and exercise and controlling blood sugar levels can help control the progression of the disease.
Injections of medication in the eye are aimed at discouraging the formation of abnormal blood vessels and may help slow down the damaging effects of diabetic retinopathy. If the disease advances, the abnormal blood vessels can leak blood and fluid into the retina, leading to macular edema. Laser treatment (photocoagulation) can stop this leakage. A laser beam of light creates small burns in areas of the retina with abnormal blood vessels to try to seal the leaks. Widespread blood vessel growth in the retina, which occurs in proliferative diabetic retinopathy, can be treated by creating a pattern of scattered laser burns across the retina. This causes abnormal blood vessels to shrink and disappear. With this procedure, some side vision may be lost in order to safeguard the central vision.
Prevention
- Blood sugar control (glycemic control).
- Blood Pressure Control—BP of less than 140/80 mm Hg for a patient with diabetes.
- Lipid Lowering—lowering LDL cholesterol through lifestyle modification. Lowering saturated fats and cholesterol, weight loss, increase physical activity, use of statins for reducing high cholesterol.
- Weight management—bring overweight is associated with increased risk of Type 2 Diabetes.

